Living with Chronic Obstructive Pulmonary Disease doesn’t mean accepting a lower quality of life. This practical guide on COPD Do’s and Don’ts gives evidence-based, easy-to-follow advice you can start using today to breathe easier, cut flare-ups, and live confidently with COPD.
Quick hook: One small change can be a big win
Imagine walking to the corner store without panting, or sleeping through the night without coughing fits. Small, consistent actions — the essential COPD Do’s and Don’ts — add up. Stick with a few simple routines and you may reduce hospital visits, improve stamina, and regain control of your day.
Understanding the why: COPD in plain language
COPD is a progressive condition (includes emphysema and chronic bronchitis) that narrows the airways and makes breathing harder. With the right strategy — medicines, breathing techniques, environmental control and lifestyle changes — many people keep symptoms manageable for years. That’s the heart of these COPD Do’s and Don’ts: practical, proven steps to protect lung function and quality of life.
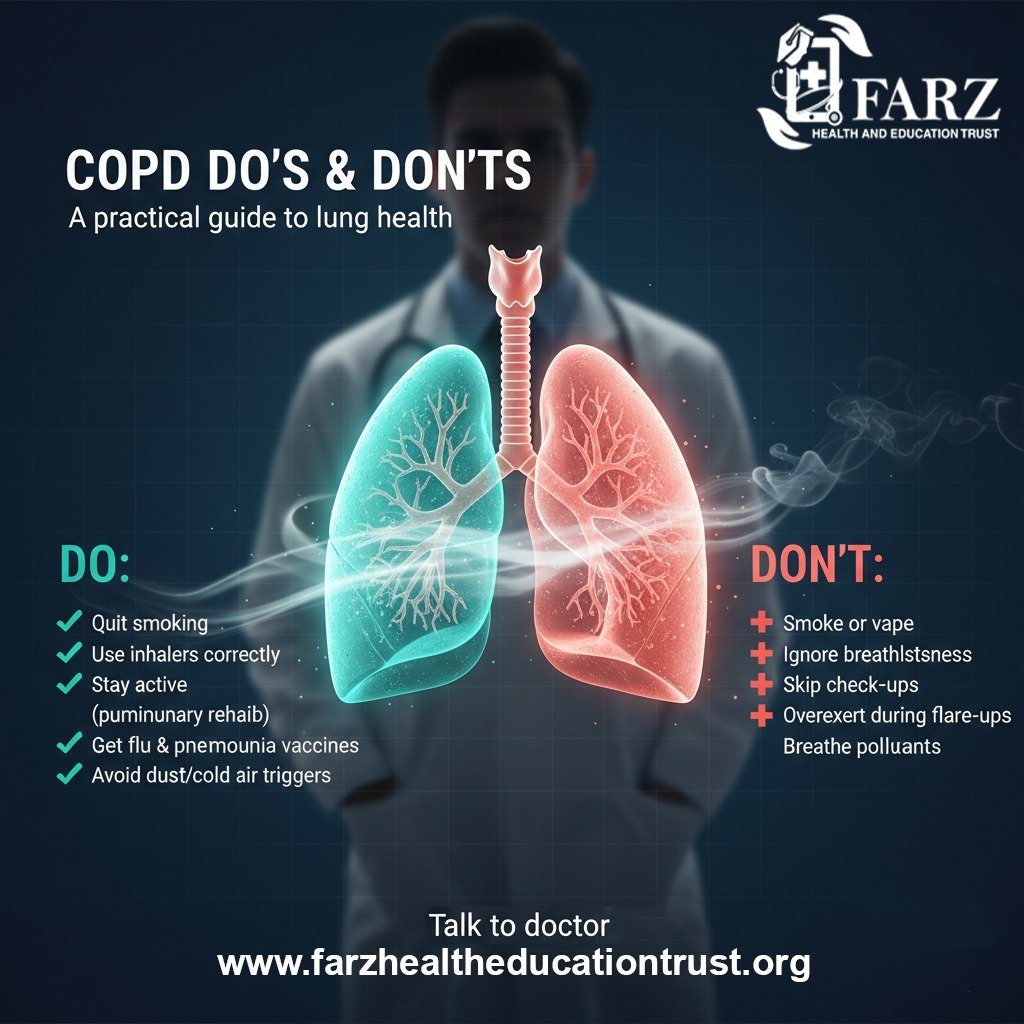
The essential DOs (what to start doing today)
1. DO follow your medication plan exactly
Adherence to inhalers and prescribed drugs is the most powerful “Do.” Maintenance inhalers prevent symptoms; rescue inhalers relieve attacks. Use spacers if recommended, check inhaler technique regularly, and set phone reminders. Correct medication use is central to the COPD Do’s and Don’ts list.
2. DO learn and practise breathing techniques
Pursed-lip breathing and diaphragmatic breathing reduce breathlessness and improve oxygenation. Practice daily—5–10 minutes—so techniques become automatic during exertion.
3. DO join a pulmonary rehabilitation program
Rehab combines exercise, education, and breathing training. It consistently improves endurance and reduces hospitalisations. Ask your pulmonologist about local or tele-rehab options.
4. DO stay physically active—safely
Aim for gentle, consistent movement: 20–30 minutes of walking, chair exercises, or stationary cycling. Muscle strength helps your breathing muscles work more efficiently.
5. DO optimise your home environment
Use HEPA air purifiers, avoid indoor smoke, control humidity (40–50%), and ventilate cooking areas. Clean bedding and reduce dust to lower triggers. These practical items belong in every COPD Do’s and Don’ts checklist.
6. DO get recommended vaccinations
Annual influenza, pneumococcal vaccines, and COVID-19 boosters (as advised) reduce infection risk and serious exacerbations.
7. DO monitor symptoms daily
Use a pulse oximeter or peak flow meter if advised, record any changes, and contact your care team early if symptoms worsen. Early action prevents hospital-level crises.
The critical DON’Ts (what to avoid)
1. DON’T keep smoking or stay around smoke
Quitting smoking is the single most important step in COPD care. Avoid secondhand smoke, wood smoke, and indoor pollutants. This is near the top of every COPD Do’s and Don’ts list for good reason.
2. DON’T skip routine check-ups or tests
Regular follow-up allows medication adjustments, early detection of infections, and timely referrals (e.g., to rehab or oxygen assessment).
3. DON’T ignore early signs of exacerbation
Worsening breathlessness, increased sputum, fever, or new wheeze can signal an exacerbation. Don’t wait—contact your doctor promptly.
4. DON’T overdo high-carb heavy meals before activities
Large meals can press on the diaphragm and make breathing harder. Smaller, balanced meals help—this practical point often appears on patient lists of COPD Do’s and Don’ts.
5. DON’T use unprescribed inhalers or stop meds suddenly
Stopping maintenance therapy or using unmonitored drugs can destabilise your condition. Always consult your clinician first.
Nutrition & weight: two sides of the same coin
Good nutrition supports breathing muscles and immunity. Aim for lean protein, healthy fats, colorful vegetables, and controlled carbohydrates. If underweight, focus on energy-dense, small meals; if overweight, gradual weight loss improves breathlessness. Include this in your personal set of COPD Do’s and Don’ts.
Mental health: don’t forget the invisible burden
COPD often coexists with anxiety and depression. Social isolation and breathlessness can amplify worry. Don’t ignore mood changes—talk to your care team, join support groups, and consider counselling. Mental wellbeing is as important as inhaler technique in the list of COPD Do’s and Don’ts.
Technology & tools to help you manage
Smartphone apps for medication reminders, telemedicine visits, portable pulse oximeters, and home oxygen concentrators (when prescribed) make day-to-day COPD care easier. Incorporate helpful tech into your routine but ensure devices are recommended by your clinician—this is one of the modern COPD Do’s and Don’ts.
Emergency preparedness: be ready, not scared
Work with your clinician to build a written action plan: which medications to increase, when to use antibiotics or prednisone (if prescribed), and when to seek emergency care. Keep an updated medication list and emergency contacts visible. Emergency planning ranks high in every practical COPD Do’s and Don’ts guide.
Practical examples of daily routines (sample)
- Morning: use maintenance inhaler, light stretches, small protein-rich breakfast
- Midday: 20-minute walk (pursed-lip breathing), hydration
- Evening: inhaler as scheduled, breathing exercises, review symptoms in a diary
Simple routines make the COPD Do’s and Don’ts manageable and effective.
Looking ahead: emerging treatments & hope
Research in 2025 continues into bronchoscopic therapies, targeted biologics, and personalised rehabilitation programs. While new treatments arrive, the everyday COPD Do’s and Don’ts—adhere to meds, avoid smoke, stay active, and monitor symptoms—remain the foundation of good outcomes.
Conclusion: make the checklist yours
The difference between a good day and a bad one with COPD often comes down to routine. Use this guide to shape your own COPD Do’s and Don’ts—start with one change this week (practice pursed-lip breathing, or book your vaccine). Small steps, repeated daily, lead to meaningful improvements in breathing and quality of life.
Ready for the next step? Print this checklist, discuss it with your pulmonologist, and make a personalized action plan. Your lungs are worth the care.
